Help our local partners realise their vision of hope for their communities
The benefit of safe male circumcision in Ugandan communities such as the Rakai District continues to show in further reduction in HIV incidence. Since commencing a large scale study in 2007, non- Muslim male circumcision has increased from 9% to 26% in 2011, with a 12% reduction in HIV incidence for every 10% increase in non-Muslim circumcision. Muslim males were not included in the study as they are circumcised at birth and the purpose of the Rakai Community Cohort study was purely to assess the effect male circumcision has as a HIV prevention tool. Efforts have also been made by the Makerere University Walter Reed Project, a collaboration between US military and scientists in Uganda’s capital Kampala, to increase safe male circumcision by developing a mobile male circumcision truck. The medical team based in this truck have carried out the procedure on more than 80 000 males in the past five years.
Such health campaigns have emerged as a result of the World Health Organisation (WHO) acquiring evidence in favour of male circumcision, which reduces the risk of heterosexually acquired HIV infection in men by approximately 60%. How circumcision confers a male added protection again HIV infection can be found on the CATIE website. WHO and the Joint United Nations Programme on HIV/AIDS recommend that ‘male circumcision should be considered an efficacious intervention for HIV prevention in countries and regions with heterosexual epidemics, high HIV and low male circumcision prevalence’.
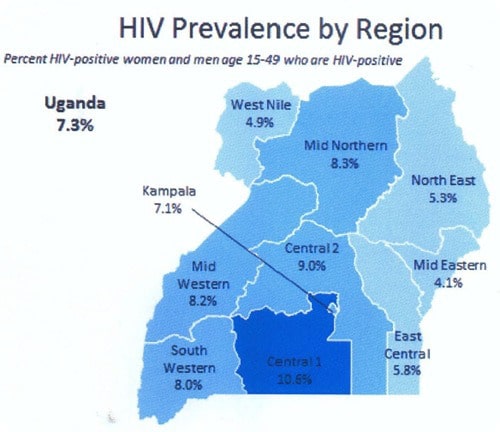
However, despite clear efforts to implement HIV health campaigns targeting males in Uganda the total HIV incidence has risen from its lowest at 6.4% in 2006 to 7.2% in 2011.
HIV incidence rise despite Uganda’s male health campaigns
Increase in HIV incidence can be attributed to lack of safe sexual practice, for example, not using condoms. AVERT, an international HIV and AIDS charity based in the UK, discovered in 2011 that only 13.7% of men used a condom when they last had sexual intercourse. This, combined with extramarital sexual activity or having multiple sexual partners is reason for the increased incidence of HIV. In 2008, the Swiss Federal Commission for HIV and AIDS released the first ever consensus statement that “An HIV-infected person on antiretroviral therapy with completely suppressed viraemia (“effective ART”) is not sexually infectious, i.e. cannot transmit HIV through sexual contact.” If not read in context with issued guidelines on how to ensure this statement remains valid for sexual partners, it is possible to believe ART medical intervention completely removes the risk of HIV infection. It is important not to misinterpret this statement otherwise HIV infection remains highly liable.
Preventing mother to child transmission- Essential in the battle against HIV
As large scale efforts have been made to reduce male HIV incidence, large scale campaigns for prevention and treatment of HIV positive women and children must follow. Moreover, it is key to prevent transmission of the infection from mother to child during foetal development and breastfeeding. WHO released new guidelines for antenatal antiretroviral therapy for HIV positive women in 2013. One mode of treatment is Option B which is the provision of ART for pregnant or breastfeeding women with CD4+ count lower than 500 or HIV infection in clinical stages 3 or 4. The results of these female targeted treatments in Uganda and other East and Sub Saharan African countries are due to be released in 2015. Only then will we be able gage efficacy of the campaign both alone and in conjunction with male HIV health targeted programmes.
Disclaimer: This blog is a space for discussion and personal reflection. Any opinions expressed within the blog are those of the author and are not necessarily held by HART. Individual authors are responsible for the accuracy of statements made within the blog.